In 10 seconds? Lynch syndrome is a hereditary condition that can increase the likelihood of colon cancer. These sorts of conditions can have important implications for cancer screening recommendations and treatments.
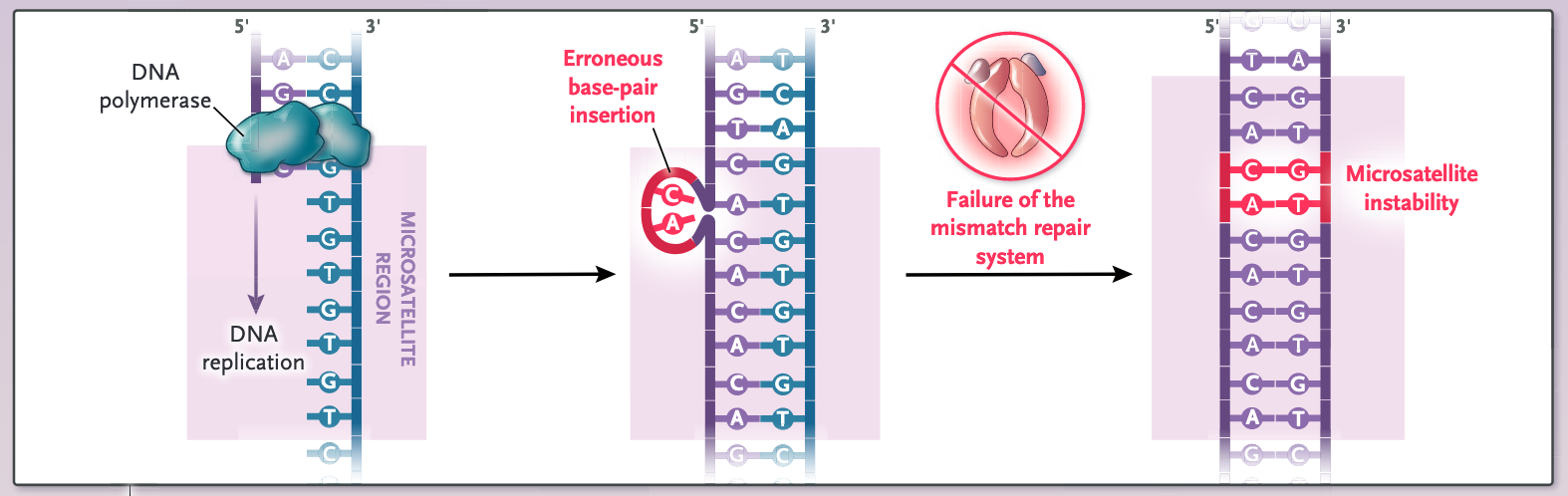
Wait, wait, could you explain how Lynch syndrome is linked to cancer? Coming right up! As a reminder, DNA serves as the operations manual for all cells in our body–dictating what all cells must do to work cooperatively. Cancerous cells undergo DNA mutations that make them grow out of sync with the rest of our cells in our bodies. In healthy conditions, cells have many safeguards to protect their DNA from accumulating mutations, one of which is the ability to fix naturally-occurring mutations in our DNA. Lynch syndrome is a hereditary condition whereby DNA repair processes are damaged (namely, a process called mismatch repair), which makes DNA mutations more likely to occur and go uncorrected. People with Lynch syndrome don't experience any symptoms but have a higher risk of developing cancer (although they could just as well live their whole lives cancer-free).
And you said it’s linked to colon cancer? Yes. Lynch syndrome is most commonly associated with colon cancer, but also can be linked (although more rarely) to endometrial, pancreatic, stomach, and other cancers. Although Lynch syndrome is only present in about 3–5% of cases of colon cancer, its diagnosis can have important implications on cancer treatment, prognosis (ie, physician estimates of patient survival and well-being), and even screening recommendations for family members.
What do you mean by implications on cancer treatment? If a cancer patient is found to have Lynch syndrome (or similar genetic defects in mismatch repair), medical guidelines dictate certain surgical, chemotherapy, or immunotherapy options (particularly the use of immune checkpoint inhibitors). The good news is that people who have Lynch syndrome-associated cancers tend to have better survival outcomes than patients with other types of colon cancer.
What does it mean for family members? First-degree relatives (siblings, parents, or children) of those with Lynch syndrome have a very high chance of having it as well, which is why they are recommended to undergo a blood test to determine their status. Relatives found to have Lynch syndrome are encouraged to undergo colon cancer screening every 1-2 years starting 5 years before the youngest age of cancer diagnosis of a family member (so if a parent was diagnosed with cancer at 40, children with Lynch syndrome would start screening at 35).
What if there are cases of colon cancer in my family but none of my relatives has been diagnosed with Lynch syndrome? Colon cancer screening is recommended for everyone starting at age 45. Screening recommendations are only modified if a family member is diagnosed with colon cancer before age 55–because the general rule is to start colon cancer screening about 10 years before the age of diagnosis of the youngest family member diagnosed with colon cancer. If colon cancer runs in your family, make sure to talk with your doctor about their screening recommendations!
Pros and Cons of Personal Genetic Screening
Personal genetic screening services, like 23andMe, although originally developed to determine genetic ancestry, have started offering cancer screening services.
While 23andMe doesn’t test for Lynch syndrome, it’s been FDA-approved for screening for some other cancer-related genetic conditions, like BRCA1/2 mutations. However, the benefit of genetic cancer screening en masse is not clearly defined.
On a positive note, results indicating a genetic risk for cancer may encourage otherwise reluctant people with genetic risks from participating in cancer screening. However, they may also spur unnecessary stress and anxiety. And since these tests don't test for all genes that increase cancer risk, negative results may instill a false sense of security.
If you're worried about your genetic risk of cancer, your best bet is to talk to your doctor or a genetic counselor!
Dr. Talia Henkle has distilled 5 papers saving you 17.5 hours of reading time.

This Science Integrity Check of this 3-min Science Digest was performed by Flávia Oliveira Geraldes